60 year old female with chronic cough with hemoptysis
Dr.ASHFAQ (INTERN)
Dr.GNANADHA (INTERN)
Dr.SRAVYA (INTERN)
Dr.CHETANA (INTERN)
Dr.NAVYA (INTERN)
Dr.VAMSHI ( PG1)
Dr.SAI CHARAN(PG1)
Dr.SUSMITHA (PG2)
Dr.ADITYA (PG3)
Dr.PRANEETH(PG3)
Dr.PRAVEEN NAIK (ASS.PROF)( duty on call 1)
Dr.RAKESH BISWAS (PROF.AND HOD) ( duty on call 2)
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Here is a case i have seen:
A 60 your old female with HF rE F with acute gastroenteritis and left bronchoalveolar pathology.
A 60 year old female came to OPD chief complaints of cough with expectoration and SOB since one month.fever since one month.vomitings and loose stools since 4 days
HOPI:
patient was apparently asymptomatic 20 years back later she had intermittent cough ( once in a month )which is relieved on taking medication but one month ago she had fever which was high grade with chills associated with low backache and SOB associated with cough with expectoration which was insidious in onset for this she went to hospital where she diagnosed with anaemia managed conservatively and she is on ceftriaxone. Symptoms aggravated more since 4 days , blood in sputum and wheeze present.
H/o vomitings since 4 days which are 4-6 episodes/ day,food and water as content,non bile stained, non blood stained.
H/o loose stools since 4 days 5-6 episodes/day.
H/o loss of appetite present.
Significant weight loss present( 4-5 kgs over the week)
No h/o burning micturition,melaena, headache.
Past history-
No history of hyperhypertension, diabetes mellitus, epilepsy,thyroid disorders, asthma, tuberculosis.
No past surgical history and blood transfusions.
- Her brother had similar complaints, died 25 years ago.
- Her sister has similar complaints chronic cough and SOB takes inhalers.
Menstrual and marital history-
Attained menarche 13 years of age and married at 14 years.
Menstrual cycles are regular 4/30,
Attained menopause by 45 years of age.
No known drug and allergies.
General examination-
PT is conscious, orientated to time, place, person, cooperative.
Thin built and Malnourished.
Skin fold thickness : 4mm.
HT-158 cm
Wt- 33 kg
BMI-13.25
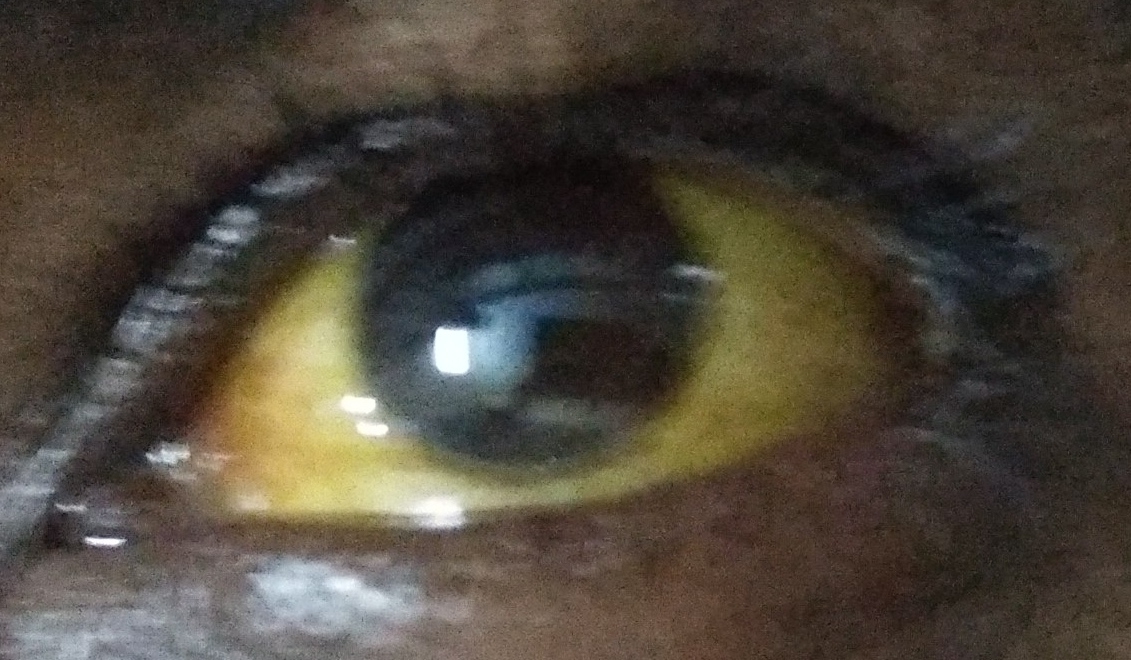
No signs of icterus,cyanosis, generalised lymphadenopathy,paedal edema.
Vitals-
Temperature-99.3F
PR- 105 Bpm
RR- 28 cpm
Bp- 100/60 mm of Hg
Head to toe Examination:
Temporal wasting present.
Shiny,bald ,bulky, red tongue.
Greyish white patch is seen over soft palate.
Muscle wasting present:temporalis, deltoid.
Ichthyotic skin present on upper limbs and lower limbs.
?hard, mobile,2.5cm left supraclavicular lymph node present.
Lower thoracic and lumbar kyphoscoliosis present.
Lower limb : significant muscle wasting present.
Saddle nose deformity +
Respiratory examination:
Inspection-
Oral cvity- poor oral hygiene- Present.
UR-:12- 45678. UL:12345678.
LR:123--- 78. LL :12---- 78.
Trachea appears to be cental.
Suprasternal pulsations present.
Trails sign+.
Deviation of mediastinal trachea to right side.
Dilated veins seen over neck,right upper anterior aspect and left hemithorax.
Barrel shaped chest.
visible pulsations present in left mid clavicular line below the nipple( 4cm).
Broadbend's sign : systolic retraction in 3 rd and 4th ICS.
Epigastric pulsations +.
On posteriorly left side lower thoracic region - ?aortic pulsations present.
abdominothoracic type respiration
Resp. movements Right. Left.
Upper zone ✓. Decreased
middle zone ✓. Decreased
Lower zone ✓. ✓
Accessory muscle usage present.
1.SCM
2.Scalenus
Palpation-
no local rise of Temperature and tenderness.
Apex beat felt over left to left mid axillary line in 5th intercostal space (4cm).
Anterioposterior diameter- 24 cm.
Transfers diameter-24cm.(APD/TD: 1/1).
Left side over crowding of ribs +.
Resp. Movements. Right. Left.
Anterior:
Upper zone. N. Decreased
middle zone N. Decreased
Lower zone N. Decreased
Posterior:
Suprascapular. N. Decreased
Interscapular. N. Decreased
Infrascapular. N. Decreased
Percussion-
Direct : resonant over clavicular, sternum.
Indirect :
Anterior. Right. Left.
Supraclavicular. Resonant. Dull
Infraclavicular. Resonant. Flat
Supra mammary Resonant. Falt
Mammary. Resonant. Flat
Inframammary. Dull. Flat
Axillary. Resonant. Dull
Infraaxillary. Dull. Dull
Posterior:. Right. Left.
Suprascapular. Resonant. Dull
Interscapular. Resonant stony dull
Infrascapular. Resonant. Flat
Auscultation- decreased air entry in both the lung areas. bilateral coarse Crepitations heard in both the lung areas.
Aegophony and bronchophony in
Right. Left
Supraclavicular. ✓ tubulobronchi.
Infraclavicular. ✓ tubulobronchi
Supra mammary A&B. tubulobronchi
Mammary. A&B tubulobronchi
Inframammary. ✓. tubulobronchi
Axillary. ✓ ✓
Infraaxillary. ✓. ✓
Suprascapular. ✓. Tubulobronchi
Interscapular. ✓. Tubulobronchi
Infrascapular. ✓. Tubulobronchi
Per abdomen-
Distended abdomen, everted umbilicus present. Distended abdominal veins.
Shifting dullness present.mild spleenomegaly.
Bowel sounds heard.
? Portal hypertension
CVS- S1,S2 heard.
CNS- NFND
Reflex's
Right. Left.
Jaw jerk. +. +
Schimizu +. +
Biceps. +++. +++
Triceps. +++. +++
Supinator. +++. +++
Finger flexor. +++. +++
Knee. +++. +++
Ankle. +++. +++
Plantar. +++. +++
Investigations-
ABG-
PH- 7.24
PCO2- 32 mm hg
Po2- 79.3 mm hg
Hco3- 13.2 mmol/L
2D echo-
Moderate TR + with PAH ,Mild MR+/AR+.
LAD hypokinesia, RCA Lcx hypokinetic ,no AS/MS.
Moderate LV dysfunction+
Diastolic dysfunction +, No PE.
USG-
B/L grade 1 RPD changes present.
ECG-
BT- 2 Min
CT- 4 Min
PR- 15
INR- 1.11
APTT- 30
Hb- 13.4
Anti HCV- Negative
HBsAg-negative
HIV1/2- negative
DENGUE- negative
Chest X ray-
Lower mediastinal shift on right side with inwardly pulled Rt Costophrenic angle.
Treatment given-
Tab. PCM 650 mg stat
Neb. With IPRAVENT 4th hourly.
Head end elevation.
On day 2
RFT-
Urea-145 mg/dl
Creatinine-1.9 mg/dl
Uric acid-10.4 mg/dl
Calcium-8.6 mg/dl
Phosphorus-3.4 mg/dl
Sodium-136 mEq/l
Potassium-4.1 mEq /l
Chloride- 102 mEq/L
2. CBNAAT-
A- 60 year old female with HFrEF ? Bronchogenic carcinoma and acute gastroenteritis with oral candidiasis.
Treatment :
Neb. With IPRATROPIUM BROMIDE 4 th hourly.
Tab. PCM 500 mg PO /SOS.
Head end elevation.
Day3
Two episodes of fever spikes present of 100.3 F.
Hemoptysis decreased.
Vomitings and diarrhoea subsided.
Treatment:
Neb. IPRATROPIUM BROMIDE 6th hourly.
Tab. EVION PO/OD.
Inj. OPTINEURON 1amp in 100 ml NS IV/OD.
Tab.PCM 650 mg SOS.
Temp charting 4th Hourly.
On Day4
C/o generalised weakness.
No fresh complaints.
O/E
Vitals
TEMP-98.8 F
PR- 104 bpm
BP- 90/60 mm of hg
RR-24 cpm
Treatment:
Neb. IPRATROPIUM BROMIDE 6th hourly.
Tab. EVION PO/OD.
Inj. OPTINEURON 1amp in 100 ml NS
Syp. GRILLINCTUS - BM 15 ml TID
Tab.DOLO 650 mg SOS
Day 5
C/o generalised weakness.
No fresh complaints.
O/E
Vitals
TEMP-98.4 F
PR- 98 bpm
BP- 100/60 mm of hg
RR-28 cpm
Treatment:
Neb. IPRATROPIUM BROMIDE 6th hourly.
Tab. EVION PO/OD.
Inj. OPTINEURON 1amp in 100 ml NS
Syp. GRILLINCTUS - BM 15 ml TID
Tab.DOLO 650 mg SOS
Day 6
Fever +, cough+
O/E
Vitals
TEMP-101F
PR- 105 bpm
BP- 110/70 mm of hg
RR-30cpm
Treatment:
Neb. IPRATROPIUM BROMIDE 6th hourly.
Tab. EVION PO/OD.
Inj. OPTINEURON 1amp in 100 ml NS
Syp. GRILLINCTUS - BM 15 ml TID
Tab.DOLO 650 mg SOS
Day7
Cough +, fever
O/E
Vitals
TEMP-101F
PR- 104 bpm
BP- 110/70 mm of hg
RR-28cpm
Treatment:
Neb. IPRATROPIUM BROMIDE 6th hourly.
Tab. EVION PO/OD.
Inj. OPTINEURON 1amp in 100 ml NS
Syp. GRILLINCTUS - BM 15 ml TID
Tab.DOLO 650 mg SOS
IVF 1unit NS. @50 ml/ hr
1 Unit RL@ 50 Ml/ hr
T3N3 M0.
Day -8
Cough +, fever subsided
O/E
Vitals
TEMP-101F
PR- 104bpm
BP- 110/70 mm of hg
RR-28cpm
Treatment:
Neb. IPRATROPIUM BROMIDE 6th hourly.
Tab. EVION PO/OD.
Inj. OPTINEURON 1amp in 100 ml NS
Syp. GRILLINCTUS - BM 15 ml TID
Tab.DOLO 650 mg SOS
IVF 1unit NS. @50 ml/ hr
1 Unit RL@ 50 Ml/ hr
Day-9
Cough +, fever present
O/E
Vitals
TEMP-101F
PR- 90bpm
BP- 80/50 mm of hg
RR-26cpm
Treatment:
INJ. AUGMENTINE 1.2 gm IV /BD( DAY-1)
Neb. IPRATROPIUM BROMIDE 6th hourly.
Tab. EVION PO/OD.
Inj. OPTINEURON 1amp in 100 ml NS
Syp. GRILLINCTUS - BM 15 ml TID
Tab.DOLO 650 mg SOS
IVF 1unit NS. @50 ml/ hr
1 Unit RL@ 50 Ml/ hr
Day-10
Cough +, fever present
O/E
Vitals
TEMP-100F
PR- 78bpm
BP- 90/60 mm of hg
RR-24cpm
Treatment:
INJ. AUGMENTINE 1.2 gm IV /BD( DAY-2)
Neb. IPRATROPIUM BROMIDE 1 resp. 6th
hourly.
Neb. BUDECORT 1 resp. 12th hourly.
Tab. EVION PO/OD.
Inj. OPTINEURON 1amp in 100 ml NS
Syp. GRILLINCTUS - BM 15 ml TID
Tab.DOLO 650 mg SOS
IVF 1unit NS. @50 ml/ hr
1 Unit RL@ 50 Ml/ hr
Day-11
Cough +, fever subsiding
O/E
TEMP-99.4F
PR- 68bpm
BP- 80/60 mm of hg
RR-24cpm
Investigations-
RTPCR - NEGATIVE
Treatment:
INJ. AUGMENTINE 1.2 gm IV /BD( DAY-3)
Neb. IPRATROPIUM BROMIDE 1 resp. 6th
hourly.
Neb. BUDECORT 1 resp. 12th hourly.
Tab. EVION PO/OD.
Inj. OPTINEURON 1amp in 100 ml NS
Syp. GRILLINCTUS - BM 15 ml TID
Tab.DOLO 650 mg SOS
IVF 1unit NS. @50 ml/ hr
1 Unit RL@ 50 Ml/ hr
Day-12
Cough +, fever subsiding
O/E
TEMP-99.4F
PR- 82bpm
BP- 90/70 mm of hg
RR-24cpm
Treatment:
INJ. AUGMENTINE 1.2 gm IV /BD( DAY-3)
Neb. IPRATROPIUM BROMIDE 1 resp. 6th
hourly.
Neb. BUDECORT 1 resp. 12th hourly.
Tab. EVION PO/OD.
Inj. OPTINEURON 1amp in 100 ml NS
Syp. GRILLINCTUS - BM 15 ml TID
Tab.DOLO 650 mg SOS
IVF 1unit NS. @50 ml/ hr
1 Unit RL@ 50 Ml/ hr
Day-13
.Cough +, fever subsiding
O/E
TEMP-99F
PR- 82bpm
BP- 90/70 mm of hg
RR-24cpm
Treatment:
INJ. AUGMENTINE 1.2 gm IV /BD( DAY-3)
Neb. IPRATROPIUM BROMIDE 1 resp. 6th
hourly.
Neb. BUDECORT 1 resp. 12th hourly.
Tab. EVION PO/OD.
Inj. OPTINEURON 1amp in 100 ml NS
Syp. GRILLINCTUS - BM 15 ml TID
Tab.DOLO 650 mg SOS
IVF 1unit NS. @50 ml/ hr
1 Unit RL@ 50 Ml/ hr